Neuropathy Symptoms and What to Do— How Podiatric Care Helps Protect Your Feet
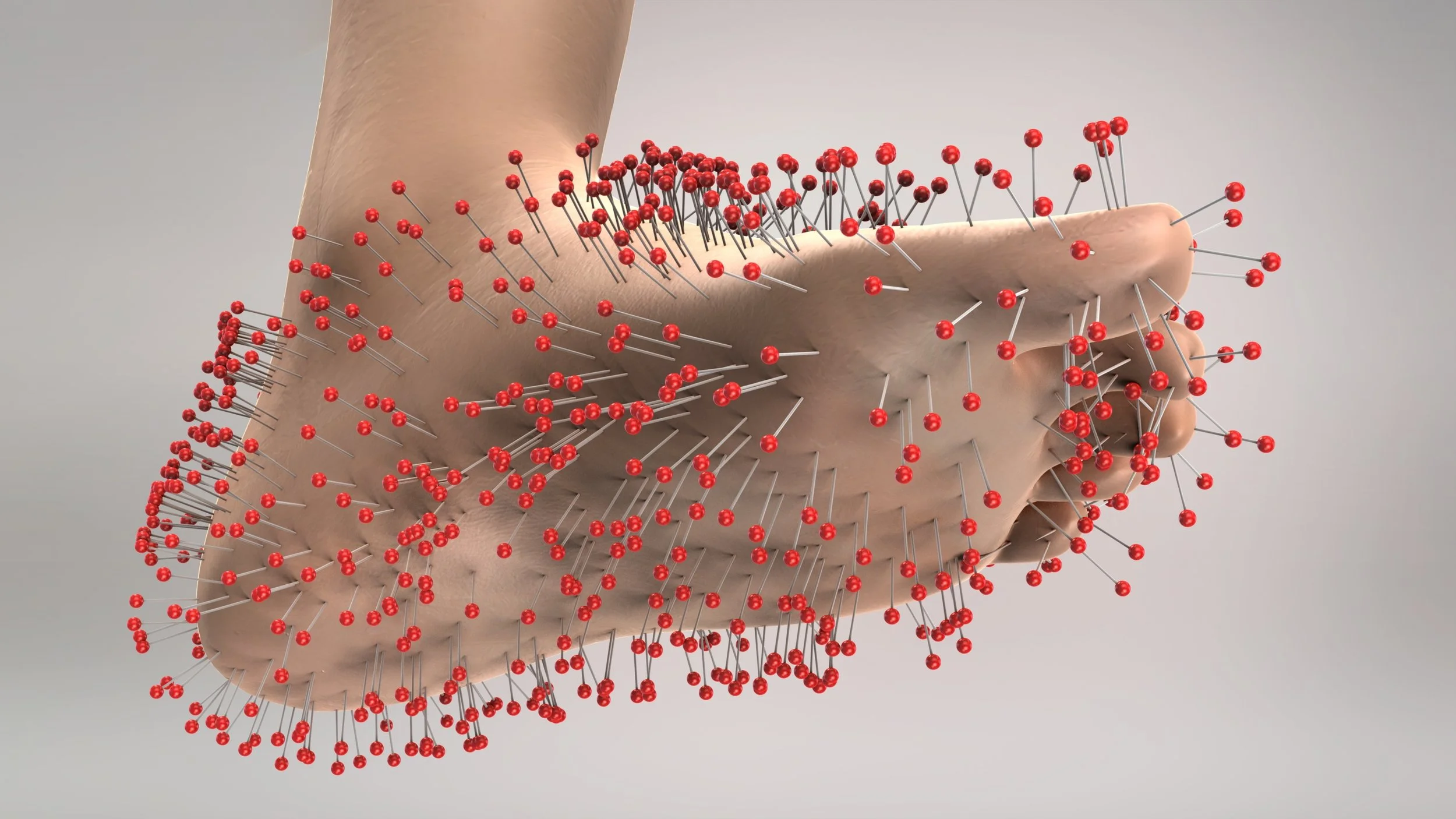
Have you ever noticed a tingling, burning, or pins and needles sensation in your feet that just won’t go away? Or maybe your socks feel bunched up when they’re not, or your shoes seem tighter than they used to be.
These subtle changes might seem like minor annoyances at first, but they can be early warning signs of peripheral neuropathy—a condition that affects the nerves responsible for sensation and muscle control in your feet and legs.
Podiatrists like Dr. Alison Young regularly see patients who have been living with numbness or discomfort for months—or even years—before realizing what’s really going on.
Understanding neuropathy’s symptoms and addressing them early can make a significant difference in maintaining your continued comfort, safety, and mobility.
At City Step Podiatry, we’re deeply invested in keeping Chicagoans healthy, happy, and moving forward. That’s why we’re committed to tackling topics of interest and importance when it comes to podiatric care and conditions that impact our feet, heels, ankles, and legs.
In this post, we’ll cover what neuropathy is, what causes it, the symptoms to look out for, when to see a podiatrist, and how podiatric care can help you manage the condition and protect your long-term foot health.
What is peripheral neuropathy?
Apart from a mouthful of medical jargon—what IS peripheral neuropathy, anyway?
When it comes to clinical terminology, many folks find it helpful to break down words into smaller parts to better understand what they mean.
Peripheral refers to something that occurs on the edge of something. You’ve likely referred to your peripheral vision before, right? That’s what you can see on the far sides of your visual field. When it comes to your body and its systems, peripheral means something that’s situated away from the center.
So, with this concept in mind, your arms, hands, feet, and legs are peripheral systems, because they’re located far from the center of your body.
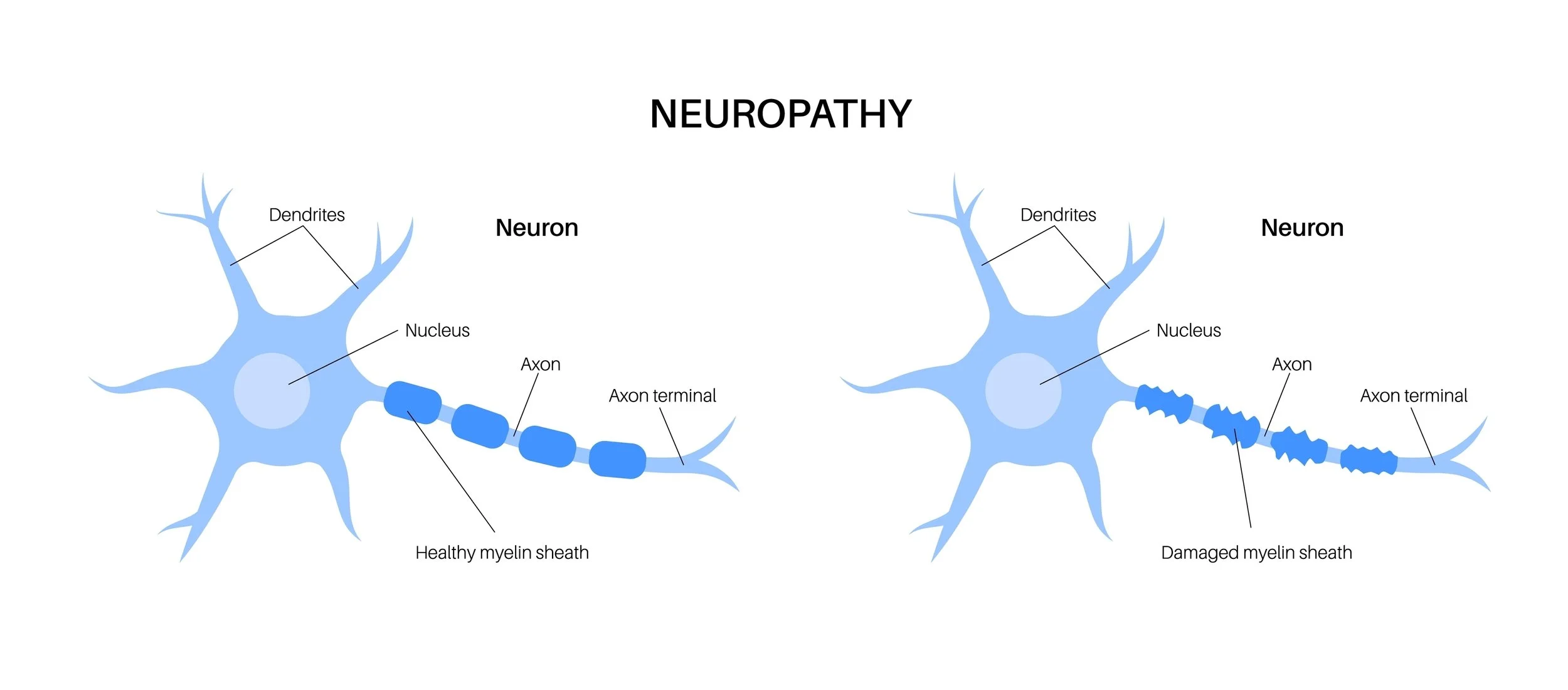
Neuropathy can be broken down into two parts. Neuro comes from the Greek word for nerve. Pathy is a suffix that denotes a disease or condition. Combine them, and you find that neuropathy refers to a condition or disease that affects the nerves of the body.
Pop both terms back together, and peripheral neuropathy becomes a disease that affects the nerves of the hands, arms, feet, and legs.
Your peripheral nerves are the network of vital nerves outside of your brain and spinal cord that transmit signals between these key central nervous system components and the rest of your body.
These nerves are responsible for both sensation (what you feel) and motor control (how you move). When they become damaged, those signals can get disrupted, leading to symptoms like numbness, tingling, or pain in the extremities, especially the feet and toes.
Peripheral neuropathy is a common condition. All told, it affects an estimated 20 million Americans.
In podiatry, we focus on peripheral neuropathy in the lower extremities, since the feet are often the first and most affected area. That’s because the nerves in the feet are the farthest from the spinal cord, making them more vulnerable to damage, reduced circulation, and slow healing.
Now that you know what peripheral neuropathy is, let’s take a look at how and why it shows up where and when it does.
Why does peripheral neuropathy affect the feet?
Your feet are a remarkable system of bones, muscles, ligaments, and nerves working in harmony to support every step you take. But because they’re at the outermost point of your nervous system, they’re also more susceptible to changes in blood flow and nerve function.
Think of it like a rural, isolated community. These places can be harder to reach with necessary supplies and services than bustling, centrally located cities.
Conditions that impact your circulation—like diabetes and vascular disease—can gradually starve your nerves of oxygen and nutrients. Over time, this chronic lack of nourishment leads to nerve damage.
Additionally, repetitive stress, poorly fitting footwear, and untreated foot injuries can worsen the problem. That’s why neuropathy so often shows up in the feet first—and why podiatrists play such an essential role in identifying and managing it early.
So, what causes neuropathy in the feet? Let’s explore some of the usual suspects.
Common causes of peripheral neuropathy
As with any complex condition, there are many possible causes of neuropathy.
Sometimes it’s linked to a clear underlying condition; other times, it develops without a single identifiable cause. In that case, you may hear your doctor refer to it as idiopathic neuropathy. This term simply means there’s no clear underlying cause for your neuropathy symptoms.
The most common causes of peripheral neuropathy include:
Diabetes: The leading cause of neuropathy. Prolonged high blood sugar levels can damage the small blood vessels that feed the nerves, especially in the feet and legs.
Alcohol use: Chronic alcohol consumption can lead to nutritional deficiencies that affect nerve health.
Smoking: Smoking increases neuropathy risks and can worsen its symptoms in those who already have it. Smoking is known to damage blood vessels, reduce blood flow, and cause toxin-related nerve damage.
Vitamin deficiencies: Low levels of vitamins B12, B6, and folate can contribute to neuropathy.
Certain medications: Chemotherapy drugs, some antibiotics, and medications used for autoimmune conditions (such as lupus) can cause nerve damage as a side effect.
Injury or trauma: Physical injuries, fractures, or repetitive stress can compress or stretch nerves, leading to localized neuropathy.
Autoimmune disorders: Conditions like rheumatoid arthritis, lupus, or Guillain-Barré syndrome can trigger nerve inflammation.
Thyroid disease, kidney disease, or infections: Chronic illnesses can also contribute to neuropathy’s development.
According to the Mayo Clinic, diabetes alone accounts for nearly half of all neuropathy cases in the United States, making routine foot checks and proactive care essential for those living with or at risk for the condition.
That’s another reason why connecting with a podiatrist you can trust is especially crucial for those dealing with chronic health conditions like diabetes.
Early symptoms of peripheral neuropathy
One of the challenges with neuropathy is that its symptoms often start subtly and progress gradually.
Paying attention to early warning signs can help you seek care before complications arise.
Common symptoms of neuropathy include:
Tingling or pins and needles sensations in the toes or soles
Burning or shooting pain, often worse at night
Numbness or decreased ability to feel touch, temperature, or pain
Feeling like you’re wearing socks when you’re not
Sensitivity to touch (even bedsheets or socks may feel uncomfortable)
Muscle weakness or a feeling of imbalance
Difficulty sensing where your feet are on the ground
As the condition progresses, feelings of numbness may increase or spread, and pain can give way to a total loss of sensation in the affected area—making it difficult to detect cuts, blisters, or injuries. This can lead to serious risks related to safety and wound healing.
Let’s explore this issue a bit more to drive home its importance.
Why early detection matters in neuropathy treatment
When neuropathy goes unchecked, it can lead to serious complications—especially in the feet.
Because sensation is reduced, sufferers may not notice small cuts, blisters, or pressure sores. Over time, these can turn into ulcers or infections that heal slowly due to poor circulation.
Loss of sensation also increases the risk of falls and balance problems, particularly in older adults. Weakness and instability in the ankles can cause tripping or missteps, which may lead to fractures or sprains.
According to research from the National Institute of Health, up to 50% of people with diabetic neuropathy may develop foot ulcers at some point. Early management and preventive care significantly reduce that risk.
Simply put: the sooner neuropathy is identified and managed, the more effectively we can prevent these complications. Thankfully, podiatrists are expertly trained to identify and help you manage peripheral neuropathy—before it seriously affects your life.
Dr. Young and the team at City Step Podiatry also proudly offer an array of state-of–the-art, personalized podiatry services and treatment approaches that are designed to keep Chicagoans healthy, active, and pain-free.
When to see a podiatrist for neuropathy
When it comes to your body, you’re the expert. You know when things are changing, even if you can’t put your finger on it.
You should never ignore changes in foot sensation or unexplained discomfort. If you notice tingling, burning, or numbness—especially if these symptoms are persistent or worsening—it’s time to schedule a podiatric evaluation.
Your podiatrist can:
Perform a thorough exam of your feet and lower legs
Test for changes in vibration, temperature, and pressure sensation
Evaluate your foot structure, gait, and balance
Identify areas of increased friction, callus formation, or skin breakdown
At City Step Podiatry, we take a proactive approach to neuropathy care. That means not only diagnosing and managing your symptoms, but also addressing the underlying factors—like footwear, biomechanics, and circulation—that influence your long-term foot health.
Speaking of footwear—be sure to follow along with our Footwear Focus blog series to get expert advice and insight into podiatrist recommended footwear options.
How podiatric care can help with neuropathy
Podiatric care plays a vital role in both managing neuropathy and preventing its complications.
A customized podiatry treatment plan for neuropathy may include:
1. Early detection and monitoring
Regular foot exams allow your podiatrist to track changes in nerve function and identify risks before they become serious and start affecting your life.
2. Protective footwear and orthotics
Properly fitted shoes and custom orthotics can relieve pressure points, improve balance, and reduce friction—helping prevent ulcers and injury.
City Step Podiatry proudly offers access to top-quality custom orthotics.
3. Foot and skin care guidance
Routine podiatric visits often include professional nail and callus care, moisturizing recommendations, and education on safe at-home routines.
Learn why professional callus care is vital for some people.
4. Balance and gait training
If neuropathy affects your stability, strengthening and proprioception exercises can help reduce the risk of falls.
5. Circulation and wound prevention
Your podiatrist can assess blood flow to the feet, identify slow-healing areas, and create a plan to prevent sores and ulcers.
6. Pain management and adjunctive therapies
For patients with painful neuropathy, options like topical medications, physical therapy, and advanced modalities may be recommended to improve comfort and nerve function.
The goal of neuropathy treatment isn’t just symptom relief—it’s preserving your mobility, independence, and quality of life.
Living well with neuropathy
While neuropathy can’t always be reversed, there’s a lot you can do to manage symptoms and protect your feet:
Here are some top tips to monitor and manage your neuropathy effectively:
Check your feet daily. Look for cuts, blisters, or color changes. If you have trouble seeing the bottoms of your feet, use a mirror or ask for help.
Moisturize regularly. Keep skin soft to prevent cracking, but avoid applying lotion between the toes.
Wear protective footwear. Choose shoes with cushioning, support, and enough room in the toe box to prevent friction. Avoid going barefoot, even at home.
Manage chronic conditions. Keep blood sugar, blood pressure, and cholesterol in check to protect nerve health.
Stay active. Gentle movement and stretching improve circulation and support nerve regeneration.
Schedule regular podiatric visits. Routine exams help your podiatrist detect early changes and adjust your care plan accordingly.
You have options in effective neuropathy management
Peripheral neuropathy may sound intimidating, but with early detection and proactive care, it’s absolutely manageable. The key is paying attention to your body’s signals—tingling, numbness, or burning are never “just normal signs of getting older.”
City Step Podiatry was founded to help our patients stay active, safe, and comfortable through every step of their foot health journey. We’re here to listen, answer your questions, and help you develop a comprehensive treatment plan that works for you.
Whether you’re experiencing new symptoms or managing a chronic condition, our team provides the support, education, and care you need to protect your feet and your independence.
If you’re noticing changes in sensation or pain in your feet, schedule an appointment to discuss things. Early evaluation is the first step toward maintaining healthy, confident movement for years to come.
You can book with us easily online or and our convenient downtown Chicago location and flexible schedule were made to accommodate busy, active people like you.
City Step Podiatry is here for you! Reach out today to schedule your visit and treat your feet to the care they deserve.