Unexplained Foot and Arch Pain? It Might Be Posterior Tibial Tendonitis—Here’s What to Know
Foot and ankle pain can be as frustrating as it is uncomfortable, especially when it seems to come and go or gets worse the more you try to stay active and push through.
If you’ve been feeling pain or tenderness along the inside of your ankle or arch, particularly when walking or standing for long periods, it’s important not to ignore these symptoms. You may be experiencing posterior tibial tendonitis.
This condition tends to sneak up gradually, which often leads sufferers to brush it off. But it can become more serious if it isn’t treated early.
Posterior tibial tendonitis is a common overuse injury that affects the tendon responsible for supporting your arch. This little tendon is tasked with a big, important job and when it becomes inflamed or weakened, the result can be pain and instability. Left untreated, it can even lead to lasting changes to the structure of your foot.
We don’t want to see that happen. That’s why City Step Podiatry is here to offer you all the insight and info you need about this issue in our latest informative blog.
With early interventions and the right support, this condition can often be managed successfully without surgery. We’ll help you pinpoint common symptoms, explore treatment options, and explain why this condition shouldn’t be ignored.
Join us as we unpack it all for you, so you can make your best, most informed foot health and wellness decisions. Let’s get moving!
What is posterior tibial tendonitis?
Let’s kick things off by exploring this condition, so you understand what it affects and why.
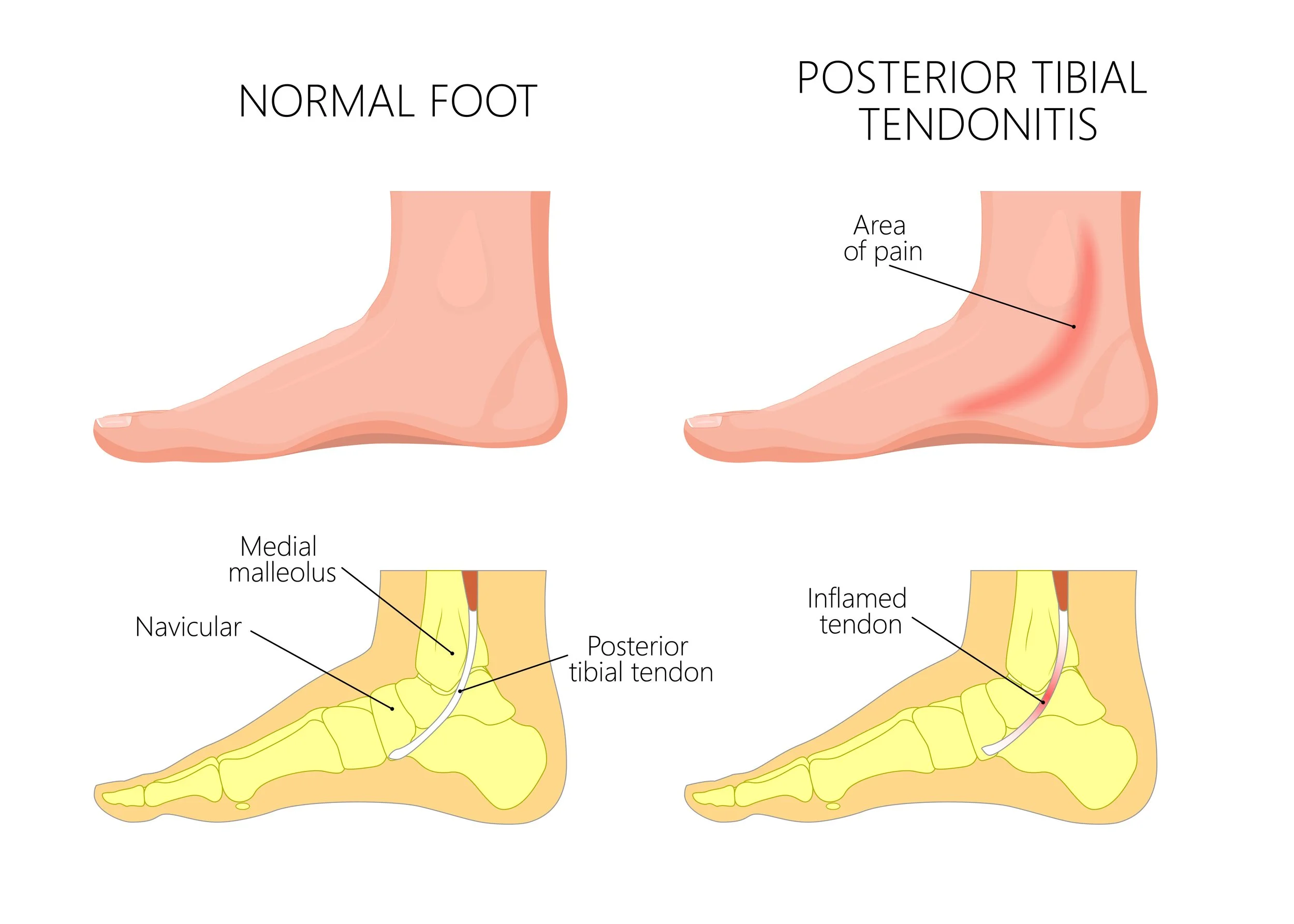
As usual, let’s get into some relevant anatomy—
Your posterior tibial tendon runs from your calf muscle, down the inside of your ankle, and into the arch of your foot.
It plays a crucial role in stabilizing your foot and maintaining the height of your arch as you walk.
When this tendon becomes inflamed or strained, it’s known as posterior tibial tendonitis.
This issue often starts gradually, with a dull ache or tenderness along the inside of your foot or ankle. The discomfort may come and go.
But over time, this condition can cause your tendon to weaken or even tear, leading to a cascade of issues—including a loss of arch support and changes in the way your foot functions.
If the condition progresses far enough, it can turn into posterior tibial tendon dysfunction (PTTD). This is a more advanced form of tendon failure that leads to flattening of the foot, difficulty walking, and significant instability.
We'll explore PTTD more below, but it’s one of the main reasons early evaluation and care from a podiatrist is so important when you’re dealing with posterior tibial tendonitis.
Common posterior tibial tendonitis symptoms
Because PTT tends to develop slowly, its symptoms are easy to dismiss at first. Paying attention to early signs, however, is vital for avoiding more serious, long-term complications.
Fear and awareness are two sides of the same coin. So, what are some clues that your foot and ankle issues may be caused by PTT?
You may notice:
Pain or swelling along the inside of your ankle or arch
Tenderness where your tendon runs behind your ankle bone
Pain that worsens with activity and improves slightly with rest
Trouble standing on tiptoe on your affected foot
A visible flattening of your arch
Ankle instability or a rolling-in sensation (overpronation)
Uneven wear on the soles of your shoes
In the early stages, you may only feel pain or discomfort after a long walk or intense workout. As the condition progresses, the pain can become more constant, affecting your ability to walk, exercise, or even stand comfortably.
What causes posterior tibial tendonitis?
Posterior tibial tendonitis is most often caused by repetitive strain or overuse.
But certain foot structures and lifestyle factors can increase your risk or enhance the strain on this vital piece of connective tissue.
Risk factors for developing PTT include:
Flat feet
Overpronation
Rapid increases in physical activity, such as starting a new walking or running routine
High-impact exercise without adequate foot support
Improper footwear, especially shoes without arch support or stability features
Obesity, which increases pressure on the arch and surrounding structures
Prior foot or ankle injuries
Inflammatory conditions, like rheumatoid arthritis or gout
Diabetes, which can impair tissue healing
Age-related changes in tendon elasticity
These factors can create more tension and strain along the posterior tibial tendon, especially during activities like walking, climbing stairs, or standing for long periods.
In addition to these risk factors, women and people with hypertension (high blood pressure) are also at slightly increased risk for PTT.
How is posterior tibial tendonitis diagnosed?
Evaluation for posterior tibial tendonitis typically begins with a detailed physical exam. Your podiatrist will assess your foot structure, range of motion, and strength, as well as check for tenderness along the tendon’s path.
They may also want to:
Observe your gait by watching how you walk
Test your ability to stand on your toes on one foot
Check for swelling, warmth, or flatfoot collapse
Palpate the tendon along the inside of your ankle
If additional clarity is needed for a clear diagnosis, your podiatrist may also order imaging studies to back up what they suspect. These may include:
Ultrasound: to detect inflammation, fluid buildup, or tendon tears
MRI: to obtain a more detailed view of your soft tissue
X-rays: to assess any structural changes, especially if flatfoot or arthritis is suspected
The earlier you can get diagnosed with PTT, the better. Early diagnosis helps prevent permanent changes and supports a faster, more complete recovery.
Since we’ve already touched on it several times, let’s now explore what can happen when PTT isn’t caught or treated early.
What is posterior tibial tendon dysfunction (PTTD)?
If posterior tibial tendonitis is left untreated—or if the tendon becomes too weakened or damaged—it can progress into a condition called posterior tibial tendon dysfunction (PTTD).
This is a more advanced stage of the condition where the tendon can no longer support the arch of the foot, leading to progressive flattening and structural deformity.
Common signs of PTTD include:
A visibly collapsed arch
The ankle appears to roll inward (also known as valgus alignment)
Pain on both the inside and outside of the ankle
Increasing difficulty walking or standing for long periods
In some cases, PTTD may lead to the inability to wear normal shoes due to foot shape changes.
PTTD is also sometimes referred to as adult-acquired flatfoot or progressive collapsing foot deformity (don’t blame us—we didn’t come up with these names!).
Once this stage of severity is reached, treatment becomes more complex and may require long-term bracing or surgical correction.
Thankfully, your podiatrist can help you identify subtle signs of dysfunction before permanent damage occurs—and build a treatment plan to keep your feet supported, aligned, and pain-free.
Posterior tibial tendonitis treatment options
Treatment for posterior tibial tendonitis depends on how advanced your condition is. In many cases, especially when caught early, conservative options are highly effective.
The overarching goal of PTT treatment is to reduce inflammation, support the arch, and give the tendon time to heal—without restricting your ability to stay active long-term.
Let’s break down the top three treatment approaches, so you can see how podiatrists conceptualize your PTT treatment journey and what you can expect.
Conservative PTT treatment approaches
Most patients in the early stages of posterior tibial tendonitis respond well to a combination of:
Activity modification to reduce strain while the tendon heals
Rest, ice, and elevation during flare-ups
Bracing or a walking boot to offload the tendon during its more painful stages
Custom orthotics to provide targeted arch support and correct overpronation.
Footwear changes, including stability or motion-control shoes
Physical therapy to strengthen the surrounding muscles and improve ankle alignment
Anti-inflammatory medications (NSAIDs), when appropriate
In-office PTT therapies
For more persistent or moderate cases of PTT, advanced non-invasive therapies can help promote healing and reduce recovery time.
Radial shockwave therapy uses acoustic pulses to stimulate blood flow, reduce inflammation, and encourage tissue repair. Learn about radial shockwave therapy.
Laser therapy delivers focused light energy to support tissue healing and relieve pain without side effects. Explore laser therapy.
Thankfully, these treatments don’t need to be painful and time-consuming. Best of all? City Step Podiatry proudly offers both cutting-edge therapeutic approaches in our convenient downtown Chicago office.
These approaches are especially helpful if you’ve tried rest and physical therapy without getting the relief you need. If you have questions, reach out to us for personalized guidance and support!
When surgery is considered for posterior tibial tendonitis
Surgery is generally a last resort in treating PTT, but it may be necessary if the tendon has partially or completely torn, or if the foot structure has been permanently altered due to PTTD.
Surgical options your podiatrist might recommend include:
Tendon debridement to remove damaged tissue
Tendon repair or transfer, using nearby tendons to restore function
Osteotomy (cutting and realigning bones) to reshape the arch
Fusion procedures in more severe deformities or arthritis-related cases
Your podiatrist will walk you through whether surgery is appropriate based on your specific symptoms, activity level, and foot structure.
The good news is, conservative treatments are usually enough for most people—but early intervention remains the best way to avoid the need for surgery altogether.
Next, let’s explore the connection between PTT and another common foot condition: plantar fasciitis.
The link between posterior tibial tendonitis and plantar fasciitis
Posterior tibial tendonitis and plantar fasciitis often go hand in hand.
In fact, part of the reason we selected this topic for this month’s information blog was because Dr. Young has been seeing a lot of PTT co-occurring with plantar fasciitis of late, and wanted to offer her valued patients some topical advice and insight into these conditions.
For more info on plantar fasciitis, check out our recent City Step blog about it.
Why are these issues connected?
Both involve structures that support the arch, and when one becomes overworked or injured, the other often compensates—leading to pain in multiple areas of the foot.
For example:
A weakened posterior tibial tendon can lead to more strain on your plantar fascia, which runs along the bottom of your foot and connects to the heel.
If you’ve already been dealing with plantar fasciitis, you may modify your gait to avoid heel pain, which can place more stress on your posterior tibial tendon.
This is why treatment often involves supporting the entire arch, addressing both tendon and fascia issues, and correcting any mechanical imbalances contributing to your symptoms.
Custom orthotics, for instance, can help by providing targeted support that benefits both conditions.
Preventing foot tendonitis and maintaining foot health
Preventing posterior tibial tendonitis means paying attention to how your feet handle everyday stress and activity.
Some tips to protect your posterior tibial tendon include:
Wear supportive shoes designed for your foot type and activity level.
Avoid sudden increases in high-impact exercise without proper conditioning.
Incorporating foot and ankle strengthening exercises into your routine.
Maintaining a healthy weight to reduce excess pressure on your feet.
Get an early evaluation if you start to notice any arch or ankle discomfort.
Taking these steps can help keep your feet strong and resilient, minimizing your risk of developing tendonitis or more serious conditions like PTTD.
Why podiatric care matters
Posterior tibial tendonitis might start as a mild annoyance, but without proper assessment and treatment, it can progress into a disabling condition.
Your podiatrist can provide a thorough evaluation, help identify early signs of dysfunction, and tailor a treatment plan that fits your lifestyle and goals.
At City Step Podiatry, our expert care includes advanced diagnostic tools and a full range of treatment options—from custom orthotics to state-of-the-art in-office therapies like radial shockwave and laser therapy. We’re here to help you not only relieve pain but also promote your mobility and protect the health of your feet in the long term.
If you’re experiencing foot or ankle pain along your arch or inside your ankle, don’t wait for the problem to worsen. City Step Podiatry is here to support you with our personalized assessments and expert treatment plans.
Take control of your foot health today with specialized care designed to restore comfort, function, and confidence.
Learn more about our insurance and flexible payment options, explore our services, and view our blog for information you can trust to make informed foot and ankle care decisions.
City Step Podiatry is here for you! Reach out today to schedule your visit and treat your feet to the care they deserve.